Imagine your heart can't do it's job beating. Blood backs up in your lungs and you feel suffocating shortness of breath, fatigue and swelling throughout your body.
This is congestive heart failure (CHF) - and it's an all too common condition that often leads to significant suffering, recurrent hospitalizations, and death.
Not surprisingly, healthy lifestyle habits including the right diet and weight management are at the core of both prevention and treatment in most cases of CHF (1).
Here's all you need to know about congestive heart failure, how to prevent it and how tackle its treatment if you or a loved one are already affected by the disease.
What is Congestive Heart Failure
CHF is a condition that develops when the heart isn’t functioning well enough to pump all of the nutrient rich blood to the rest of the body.
It’s estimated that as many as 1 out of every 5 people will develop heart failure at some point during their lifetime. Almost 6 million people have heart failure and it’s estimated that half will die within 5 years of their diagnosis (1-2).
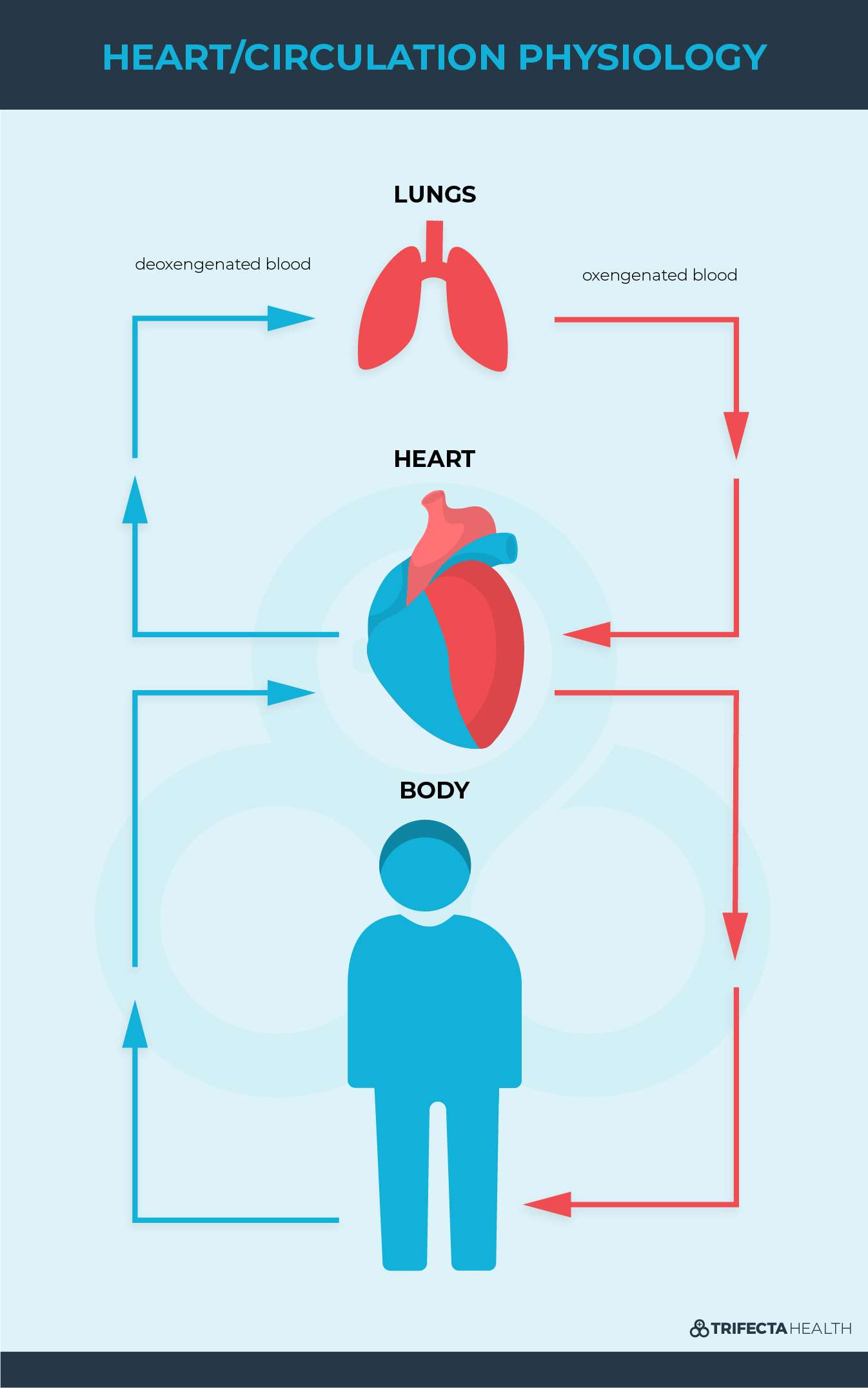
To understand this better, let’s start with some basic anatomy.
Our heart is in charge of delivering precious oxygen and nutrients to all of our organs by pumping blood throughout our body. Blood flow travels from our legs and body to the right side of the heart, then to the lungs, to the left side of the heart and then back to the rest of our body.
The amount of blood the heart pumps out is called the ejection fraction (EF). More advanced heart failure stages have lower ejection fractions.
If the heart isn’t pumping in the right way, this circulation stops working as well as it should and causes fluid to accumulate where it shouldn’t. This causes many problems. For example, when this fluid accumulates in the lungs it causes people to have difficulty breathing; and when it gets stuck in the legs it causes swelling.
Congestive Heart Failure Definition
Congestive heart failure is a general term that refers to the heart being unable to effectively pump blood. However, you may come across more specific terms when talking about heart failure. There can be right sided heart failure, left sided heart failure, diastolic heart failure, systolic heart failure - or any combination of the above.
Diastolic Heart Failure
Diastolic heart failure refers to a problem with the hearts ability to relax to allow enough blood to enter it between each heartbeat. This can be thought of as a heart that is too stiff or rigid. No matter how good it is at squeezing, the heart can’t pump enough blood to the rest of the organs if not enough is able to enter in the first place.
Right Sided Heart Failure
Right sided heart failure refers to a problem with the right side of the heart. The right heart pumps blood to the lungs to become oxygenated. When there's a problem with how well the right side of the heart pumps blood, fluid begins accumulating in the rest of the body - like in the legs and abdomen.
While there are many causes of right sided heart failure, the most common cause is left sided heart failure. This is because the right heart becomes strained when not enough blood is pumping through the left side.
Systolic Heart Failure
Systolic heart failure means the heart isn’t squeezing strongly enough to push blood through the rest of the body.
Left Sided Heart Failure
The most common initial problem in heart failure is with the left side of the heart. This leads to fluid backing up into the lungs causing people feeling short of breath. It also makes the right side of the heart work harder and will cause right heart failure if not treated.
Congestive Heart Failure Symptoms
Common symptoms of CHF include:
1) Shortness of Breath
A hallmark of congestive heart failure is shortness of breath. Because the difficulty breathing is caused by fluid in the lungs, shortness of breath usually gets worse when people lay down flat - as this allows the fluid to spread out across the lungs.
Fluid accumulating in the lungs creates such significant shortness of breath that it leads many people with CHF to sleep on multiple pillows at night, or sometimes even sleep sitting up. It also limits many people from doing activities they want to do.
2) Swelling
When the right side of the heart also stops working well, fluid backs up even further - accumulating in the abdomen and/or legs. You may hear your doctor call this “pitting edema” because when you push on the swelling it leaves an indentation or ‘pit’ on the skin for a few seconds (sometimes longer) before filling back up with fluid. This also often leads to weight gain.
3) Generalized Fatigue & Weakness
When the heart is functioning poorly people often experience fatigue and sometimes generalized weakness. It may be harder to engage in activities they used to, or simple walks and exercise because of this generalized fatigue, in addition to the shortness of breath.
4) Irregular Heart Beat
CHF can cause an irregular heart beat, most commonly atrial fibrillation. This can be uncomfortable by causing heart palpitations, generalized weakness, shortness of breath or chest pain. It can also be dangerous by leading to other problems like stroke.
Congestive Heart Failure Stages
Because there can be such a significant variability in the severity of CHF symptoms, the disease has been divided into different stages that were initially established by the New York Heart Association. The quality of life decreases at higher stages.
Stage 1 Heart Failure
This is the earliest stage of heart failure. People in this stage may not yet experience symptoms, even though their heart isn’t working quite as well as it should be.
Stage 2 Heart Failure
As heart failure advances, people begin to feel symptoms (like shortness of breath or fatigue) with exercise.
Stage 3 Heart Failure
The next stage of heart failure progression involves feeling badly with any physical activity. This includes basic daily activities like walking to the bathroom or getting dressed.
Stage 4 Heart Failure
Heart failure quickly consumes the lives of affected individuals in the most advanced stages. People suffer from symptoms even while resting. They may need to use a machine to help them sleep at night (CPAP or BiPAP) and they aren’t able to tolerate most physical activity.
American Heart Association Heart Failure Classification (4)
|
A |
At high risk for heart failure but without structural heart disease or symptoms of heart failure. |
|
B |
Structural heart disease but without signs or symptoms of heart failure. |
|
C |
Structural heart disease with prior or current symptoms of heart failure. |
|
D |
Refractory heart failure requiring specialized interventions. |
Congestive Heart Failure Life Expectancy
The life expectancy for someone with CHF is extremely variable depending on how advanced their disease is, the other medical problems an individual has, and how compliant they are with treatment (5).
Without treatment, it is estimated that only 60% of people in Stage 2&3 will survive the upcoming 4 years and only 40% of people in stage 4 will survive the following 12 months (6).
Congestive Heart Failure Causes
The good news is that most causes of congestive heart failure are within our power to change by altering our diet and lifestyle. Working to prevent the development of or aggressively treat the below conditions is key to preventing and treating most causes of CHF.
1) Obesity
People who are overweight are more likely to develop heart failure. Many of the other common risk factors described below also more commonly occur in people who are overweight or obese. Therefore losing weight not only decreases the independent risk factor of obesity, but it also lowers the chances of developing (and can help to treat) many of the other important risk factors for CHF below including diabetes, hypertension and coronary artery disease.
2) Diabetes
Diabetes is another risk factor for CHF. The mainstay of treatment for diabetes involves keeping blood sugar controlled with as little fluctuations as possible by eating the right diet, exercising and taking medications regularly when prescribed by your doctor.
3) Heart Disease
Other forms of heart disease also place people at an increased likelihood of developing CHF. Examples of these include cardiomyopathy (heart muscle damage), myocarditis (inflamed heart muscle) and congenital heart disease (heart disease you’re born with).
4) Coronary Heart Disease
Coronary heart disease occurs when the blood vessels in the heart are clogged. This prevents the heart from getting enough oxygen. When there’s too little oxygen being delivered to the heart muscle for too long, the tissue can die resulting in what you may know as a ‘heart attack’. Coronary artery disease is caused by many of the same things congestive heart failure is - including being overweight, diabetes, hypertension and smoking.
Valvular Heart Disease
Valvular heart disease means there’s a problem with the valves in the heart - and it can develop in a variety of ways. Some people are born with these conditions. If you have been diagnosed with a heart valve problem it’s important to follow closely with your doctor to make sure it’s not getting worse and to prevent congestive heart failure from occurring. Sometimes these valves are replaced if they are causing problems and in some cases this can help to prevent or treat CHF and other associated conditions.
5) Hypertension
Another risk factor for CHF is high blood pressure. Keeping your blood pressure consistently controlled by eating the right diet, exercise, taking medications as prescribed and regular blood pressure checks decreases the risk and progression of CHF - as well as other dangerous conditions like stroke.
6) Smoking
Smoking is another major risk factor for many conditions - including CHF, hypertension and coronary heart disease (in addition to a wide variety of cancers of course). Committing to stop smoking will benefit your health in a myriad of powerful ways.
7) Illicit Drug Use
Drug abuse - especially stimulants like cocaine and methamphetamines - are extremely hard on the heart and frequently lead to CHF.
8) Other Causes
Other diseases and hereditary conditions are much more rare causes of heart failure (ie: HIV, amyloidosis, hyperthyroidism, and hemochromatosis)
Congestive Heart Failure Treatment
Prevention and aggressive early treatment are key. The earlier you start changing your lifestyle and minimizing these risk factors, the better it your body will be.
1) Congestive Heart Failure Diet
Eating the right diet is a big part of treating CHF. The key concepts to remember when modifying your diet to help prevent and treat heart failure include minimizing salt intake and limiting calorie intake to achieve weight loss. This also helps to prevent other health ailments related to diet and obesity including high cholesterol, stroke and atherosclerosis.
Minimize Salt Intake
A diet high in salt is bad for CHF because the salt you consume brings with it water that increases the total amount of fluid the heart is required to pump. A low salt diet helps to reduce the total amount of fluid impacting the heart. A low salt diet is also critically important for treating hypertension - which when controlled further helps to prevent and treat CHF.
Calorie Control
Controlling calories for a goal of weight loss and eating heart healthy foods like whole grains while minimizing processed and fried foods is paramount to heart health.
2) Exercise
Exercising not only benefits the heart by contributing to weight loss, it also helps it to intrinsically work more efficiently. Just like any muscle, the heart gets stronger with proper use. ‘Cardio exercise’ or exercise that increases your heart rate through activities such as walking quickly, running, biking, and swimming all have a tremendous positive effect on your heart health.
3) Heart Failure Medications
There are many medications for heart failure that your doctor may prescribe for you. Common medications for heart failure include lasix (‘water pill’), beta blockers and ace inhibitors.
A common side effect many people don’t like is the increased urination (frequent peeing) that is associated with some of the medications for CHF. It’s so important to continue taking these medications as prescribed despite these annoyances because the act of peeing is what helps to remove the fluid from the body and helps the heart pump more effectively.
While none of these medicines can cure heart failure, their goal is to help prevent it from getting worse. Some of these medicines may be targeting the fluid overload itself and can work to help decrease the total fluid in the body while others may be prescribed to you to help prevent and treat the other conditions described above (ie: hypertension, diabetes, coronary artery disease) all of which can make CHF worse.